Do you struggle with painful periods that seem to be getting worse over time? Despite what you may have been told, period pain isn’t something you should just accept. It could be a sign of an underlying condition called Endometriosis.
Many women are taught from a young age that period pain is normal and are advised to manage it with heat packs, pain medications, or the oral contraceptive pill. However, what’s often considered “normal” period pain can actually be a sign of Endometriosis—a chronic inflammatory condition that can worsen and even lead to infertility if left untreated.
Did you know that 1 in 10 women are diagnosed with Endometriosis, with an average diagnosis time of 6.5 years (down from 7-12 years)?
In this blog, we’re dedicated to shedding light on the signs and symptoms of this challenging condition and offering a naturopathic and nutritional approach to managing it.
What is Endometriosis?
Endometriosis occurs when tissue similar to the uterine lining, which typically sheds each month to create your period, grows outside the uterus. This endometrial-like tissue can appear on the ovaries, fallopian tubes, cervix, rectum, bowel, and bladder. In some cases, it has been found in more distant locations, such as the lungs, diaphragm, spleen, gall bladder, stomach, and even the breast.
During your period, the normal uterine lining sheds as usual, but the misplaced endometrial tissue also breaks down in the pelvic cavity. This can lead to inflammation and pain, and may result in painful adhesions and scarring.
Common Symptoms of Endometriosis
Endometriosis is an inflammatory condition that can present with a wide range of symptoms, depending on where the endometrial tissue is located. The most debilitating symptom is often pain.
You might experience:
- A heavy or dull dragging sensation in the pelvis before your period, caused by progesterone increasing the volume of endometriotic tissue, often accompanied by bloating.
- Sharp, cramp-like pain during your period.
- Severe pain that can lead to fainting, vomiting, and diarrhoea.
- Pain during sex.
- For those with stage 3 or 4 endometriosis, pain when passing a bowel motion or urinating, due to endometrial tissue affecting the bowels or rectum, typically experienced during your period.
Other common symptoms of Endometriosis include:
- Heavy periods
- Bleeding between periods
- Bloating
- Nausea
- Difficulty conceiving
What Causes Endometriosis?
The exact cause of Endometriosis remains unclear, but several theories offer insights into potential drivers of the condition. Some theories are long-standing, while others are based on emerging research:
1. Retrograde Flow
This theory suggests that menstrual blood flows back into the pelvis instead of exiting through the vagina. Women with blockages that restrict menstrual flow, such as congenital abnormalities, adhesions, or an intact hymen, may have a higher incidence of endometriosis. Additionally, painful periods with stronger uterine contractions can increase retrograde flow.
2. Inflammation
It’s uncertain whether inflammation causes Endometriosis or if it results from the endometrial lesions, or if it’s a combination of both. Women with endometriosis generally have higher levels of inflammatory markers, which can promote the growth of endometrial cells.
Treating and managing the inflammation is absolutely essential to improve the debilitating symptoms associated with endometriosis.
3. Oestrogen Excess
Elevated oestrogen levels can stimulate a thicker endometrium, leading to heavier menstrual flow and increased risk of pelvic contamination. Moreover, endometrial lesions themselves can produce oestrogen locally, which exacerbates pain and inflammation.
4. Unhealthy Vaginal and Gut Bacteria
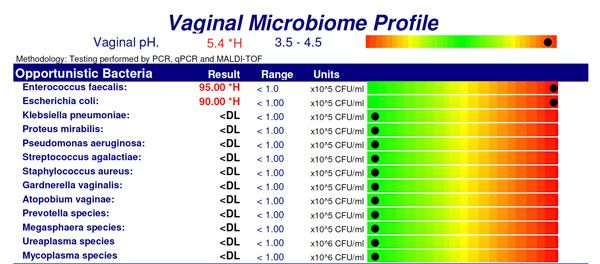
Higher levels of gram-negative bacteria have been found in the vaginal ecosystem and digestive systems of women with endometriosis.
This ‘microbial hypothesis’ suggests that bacteria may migrate from the vagina, or digestive system to the pelvic cavity due to intestinal permeability (leaky gut syndrome), driving inflammation.
5. Autoimmunity
It’s challenging to determine whether an autoimmune response drives endometriosis or if it’s a result of the endometrial lesions. However, several studies have reported the presence of auto-antibodies targeting endometrial tissue.
Understanding these potential drivers can help in managing and treating Endometriosis more effectively.
Dietary and Lifestyle Risk Factors Associated with Endometriosis
- Alcohol Consumption: Studies indicate that women with Endometriosis tend to consume more alcohol compared to those without the condition. Although the exact reason isn’t clear, high alcohol intake is known to increase oestrogen recirculation and promote inflammation and dysbiosis (bad bacterial overgrowth) in the digestive system.
- Caffeine Intake: Women who consume more than 2 cups of coffee or 4 cups of tea per day face a greater risk of infertility associated with Endometriosis.
- Sex During Menstruation: An American study found a correlation between Endometriosis and engaging in intercourse during menstruation.
- Tampon Use: While tampon use is not strongly linked to Endometriosis, a connection has been observed with long-term use (over 14 years).
- Intense Physical Activity: Engaging in strenuous exercise during menstruation may heighten the risk of Endometriosis, potentially due to increased retrograde flow of menstrual blood into the pelvis.
Treating the Root Cause: A Naturopathic and Nutrition Approach
Though the gold standard treatment for Endometriosis is successful excision of endometrial lesions, 30% of women can experience a recurrence of endometriosis with in 5 years after surgery.
When supporting women with Endometriosis, our focus is on identifying and addressing the underlying factors contributing to the condition. Our approach includes:
- Assessing the Gut Microbiome: We evaluate if there is an overgrowth of gram-negative bacteria that might be migrating to the pelvic cavity and contributing to Endometriosis. If necessary, we aim to restore a healthy balance between good and bad bacteria, often recommending a Complete Microbiome Map to assess digestive health.
- Improving Oestrogen Clearance: We support the liver and bowel in clearing excess oestrogen through targeted dietary recommendations and herbal medicine.
- Supporting Healthy Progesterone Levels: We work to balance progesterone levels to counteract oestrogen excess.
- Reducing Inflammation: We use dietary adjustments, exercise, and herbal medicine to help manage inflammation.
- Considering Food Sensitivities: We evaluate sensitivities to casein and gluten, which may exacerbate autoimmune responses.
Ready to find relief and address Endometriosis holistically?
Our team at Embodii is here to support you every step of the way. Book your initial consultation today and let us help you take control of your health and well-being. Contact us now to start your journey towards a more balanced and less debilitating menstrual cycle.












